Monday, October 12, 2009
AAFP Congress of Delegates Experience
Thursday, October 8, 2009
Some Recent News from AAFP
Upcoming Events!

We have super exciting events lined up for the next few weeks, especially as we partner with other student organizations to host National Primary Care Week together. This year's theme is:
The Future of Medicine is Now
October 19-23, 2009
Dr. Epperly will begin the evening as the keynote speaker. He will be addressing the key role of family medicine and primary care in serving the future of health care in America, with a focus on minority health issues. He will also be discussing current health care reform efforts.
His keynote will be followed by dinner, small group discussions on advocacy, and networking opportunities. We hope everyone will be able to make this talk-- it is certainly not often that BUSM gets a visit from the president of a national professional academy, and even rarer to have that guest be so well-versed in and intimately connected to the current healthcare reform debate with a powerful voice for primary care and for family medicine.
Monday, August 24, 2009
Sports Medicine Workshop: On Field Emergencies
Hope you had a good weekend! You are invited to our first Sports Medicine Workshop of the year -- limited to the first 20 RSVPs. Look out for the sign up email in your inbox soon.
- Who: Everyone!
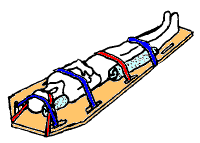
- What: What is Sports Medicine? Introduction to On Field Emergencies! Dr. Alysia Green will be discussing the field of Sports Medicine. She will also be teaching us how to handle on field emergencies and how to spine board an athlete/patient!
- When: Thursday (8/27) 5:30pm (will end no later than 7:30pm)
- Where: L-301
- Why: Learn about sports medicine, practice spine boarding on each other, meet first and second years, and eat snacks!
Thursday, August 20, 2009
Contact Info from the Lunch Panel
Also, we received some great questions about Family Medicine from your feedback evaluations. We will write a whole separate post to answer as many as we can, so keep visiting the blog!
Here are the email addresses of our panelists from Tuesday who all agreed that they would be happy to respond to questions you might have:

- Dr. Markuns (International Health interests)- Jeffrey.Markuns@bmc.org
- Dr. Green (Sports Medicine interests)- Alysia.Green@bmc.org
- Dr. O'Brien (Ob-Gyn/Rural health interests)- michlynn@bu.edu or Michelle.OBrien@bmc.org
- Anthony Lim (BUSM IV) - alim@bu.edu
- Christopher Simons (BUSM IV)- simonsch@bu.edu
LeBoHA program
Libby Cunningham is the Program Coordinator (ecunning@bu.edu)
Dr.Markuns also mentioned that students should feel free to contact him directly with further questions.

Wednesday, August 19, 2009
Sports Medicine Workshop series!
This year's workshops will all take place on Thursday evenings, 5:30-7:30pm. Because the workshops teach hands-on skills, each workshop will be limited the first 20 students to sign up. Emails will be sent out in advance of each workshop with specific RSVP links. For those who like to plan ahead, check out the FMIG Events calendar at the top right corner of this page to see all upcoming Sports Medicine Workshop dates and topics.
*** The first workshop is next THURSDAY 8/27. Dr. Green will introduce Sports Medicine, in the context of Family Medicine, and will teach spine boarding! ***
Donna (MS2, kurowski[at]bu.edu) works closely with Dr. Green to plan these workshops throughout the year. Email her if you have any questions!
Monday, August 17, 2009
Reminder about AAFP
What is Family Medicine? Lunch Panel TOMORROW!
- Who: Everyone
- What: What is Family Medicine? Hear from family physicians and a 4th year student applying to family med residencies.
- When: Tuesday (8/18) 11:30am-12:30pm
- Where: L-110
- Why: Learn about the full scope of practice in family medicine, meet first and second years, and eat free PIZZA! (Hint: always better to come early when there's free food...)
Back to School

Some of the FMIG leaders: Donna, Neetu, Lucas, and Jessica
(Not pictured: Carly, Caitlin, Erkeda)
Last Thursday, a group of second year students including many of the FMIG leaders volunteered at a health fair hosted by the Codman Square Health Center, a popular CCHERS site. We took blood pressures, spoke with teenagers from the community who helped to run part of the fair, and generally helped out where we could.
Carly also discovered that many of the teens there were part of an awesome local organization called BOLD Teens committed to improving the quality of life in their Dorchester neighborhood. It was pretty cool to hear about what that group has accomplished over the years, and to see the investment and involvement they have in their community. I have to admit that I have not explored Boston enough yet, nor spent enough time in some of Boston's neighborhoods. Many of the family medicine faculty at BMC have their clinics at community health centers, and so much of their practice is getting to know the residents of that community. I hope we all have more chances this year to venture beyond the BUSM bubble!
Monday, August 3, 2009
Messages about NC09 from a newbie
As someone who was interested in FM, and now even more so, I think it was a great way to meet folks with similar questions, ideas for career paths, as well as folks with different ideas that I didn't think could/would work but clearly can in FM!
The residency fair was amazing, and a bit overwhelming, but since it's FM, everyone was super nice, friendly and supportive of what I was interested in even if it was not what their school offered. As an MS3 going to the residency fair, it was helpful in sorting out which programs I wanted to try to contact for possible sub-i's, and which programs I could spend more time researching. The fair also gave a good idea of what the people are like at that residency program. The diversity, the mentality, the focus, the spirit-if you will-of the programs.
Plus one gets to tote home a boatload of goodies: brochures, pens, gadgets, bandaids, stressballs etc and most importantly, contact info!
The workshops are also quite good: useful and applicable even if you are not necessarily interested in FM. I attended the Wilderness Medicine (sponsored by our friends up in Central Maine--they're awesome!!!), Dermatology, Maternal/Childbirth/OB, Applying to Residency workshops. All were helpful in dispelling some myths, providing more ideas, and all in all being useful info to have.
Last thing: Midwest airlines has a hub through Milwaukee. BUT, they serve 2 fresh baked, piping hot chocolate chip cookies on every flight! And the Aladdin hotel (Holiday Inn) rocks the champaigne and the retro-cool and definitely wins in terms of hotels.
Tips for next year (MS4): stay the whole time, bring business cards, CV, personal statement, nicer outfit, and your best smile.
Sunday, August 2, 2009
Congress of Students and Continuity of Care
At the beginning of July, I was recruited to serve as a member on a Reference Committee and began my journey in the Student Congress world of the National Conference. Concurrent to the workshops and exhibits, 50 delegates (from each state) and other interested students convened in the AAFP student government/congress Thursday thru Saturday. The congress serves two purposes: to write resolutions and to elect student leaders. I will speak here about the resolution writing process.
In the first session, a brief overview of the resolution writing process was discussed followed by discussion groups based on topic. I attended the education/career planning discussion group because one of the issues I am passionate about is continuity of care education opportunities in medical school. Looking at my school's clinical curriculum, I lament the fact that there are no continuity experiences available to students. We spend between 4-6 weeks at each site and at most see patients twice. I think that continuity experiences would allow medical students to realize the value of primary care and I spent much of my first few weeks in clerkship dreaming about a weekly continuity clinic and decided I would submit a resolution on this issues.
My resolution is as follows:
"Medical Education Continuity of Care Curriculum Recommendations
Whereas continuity of care is an esteemed value of the practice of family medicine, and
Whereas early exposure to continuity of care experiences during medical school may increase interest and awareness of family medicine as a potential career choice, and
Whereas continuity of care is beneficial to patients and enhances health outcomes, be it
Resolved, that the American Academy of Family Physicians recommend to the Council of Academic Family Medicine to explore creating curriculum recommendations to incorporate a longitudinal continuity of care experience throughout medical school such as a 4-year weekly continuity clinic."
After submitting the resolution, it went to a reference committee. Reference committees listen to testimony about the resolutions from authors and other interested parties, study proposed resolutions and provide recommendations to the congress for adoption of resolutions. They function to reduce the time needed in congress. As such, congress reviews the recommendations of reference committees and only opens individual resolutions when requested.
In addition to submitting a resolution, I also served as a reference committee member for the first time. In this position, I listened to testimony about resolutions, reviewed the resolutions with the rest of the committee and made recommendations for the congress. It was very encouraging to see that medical students were very engaged and passionate about issues surrounding family medicine. Proposed resolutions ranged from developing sleep disorder curricula to health care reform position proposals to changes in web design in the AAFP website.
This was my first time participating in the parliamentary procedure to pass resolutions and elect student officers. I thought that it was a very enlightening experience! Also, my resolution was passed both by the reference committee and in congress, and will make its way to the Council of Academic Family Medicine (composed of FM dept chairs) where hopefully they will develop curricular recommendations and guidelines for longitudinal continuity experiences!
Saturday, August 1, 2009
Massages from the AAFP
Let your voice be heard! - Advocacy in Family Medicine
One student said she had never really been excited about advocacy until she stepped back and looked at the big picture of how many people she could reach with her actions. She also reminded us not to be intimidated by people at your elected representative's office and to recognize the value of speaking with the staff there even if you can't speak to your senator or congressperson.
One of the residents explained his theory of advocacy through research; performing research with the intention to change policy or viewpoints on a particular subject with your outcomes. He also reminded us that advocacy was all about "making noise" wherever you can, whether it is presenting your research results to the local news station, writing a letter to the editor of your local newspaper or serving on a committee of the AAFP, AMSA etc.
Another student reminded us that we all already advocate for our patients everyday, and that taking the next step to advocate for groups of patients is not too big a step for a student. Taking a leadership role in your local chapter of the AAFP might be a good first step or coming to the national conference and participating in the business sessions.
Another resident provided some helpful advice for getting started, including: find an organization whose "voice" you agree with and start showing up to meetings, don't be afraid to take on tasks and make your voice heard when asked, and be on the look out for people who come into your life and inspire you to change your vision or goals.
My thought it that, as physicians, we are going to be looked upon as leaders whether we like it or not, so it behooves us to be prepared with the knowledge (and hopefully practice) of how to advocate for change when it is necessary.
A little bit about me:
I am a 4th year at BUSM applying in family medicine this year. I was one of the co-leaders of the FMIG during my second year and have been a FaMeS member since 1st year. I am currently the student director sitting on the Massachusetts Academy of Family Physicians' Board of Directors.
If anyone out there is looking for more information about how to get involved either at the state or national level with the AAFP, please email me at simonsch@bu.edu
Ready to Start School Again...

The conference has officially ended by now, though I had to miss most of the last day due to an earlier flight. I have to admit that I did not have many expectations when I first arrived in Kansas City just a couple days ago, largely because I was still enjoying my Last Summer Vacation too much to think about medical school stuff. Now, I am so glad I went to AAFP's National Conference right before starting second year. The gears in my head are creaking back to life, and I couldn't help but send out a few emails to my fellow FMIG leaders to share the excitement!
(Excitement about FMIG, not about the upcoming exams every three weeks during second year.)
I learned so much more about what it means to be a family physician this week. And I would write more, but it's landing time at Logan!
UJC (Ultimate Journal Club)
In the article, Dr. Stange narrates a patient story in which issues of transition of care, physician-patient relationship, and continuity of care significantly impact the life (and health) of a person in his care. He notes that the generalist is uniquely able to address these issues, and is distinguished by the following characteristics (among others):
- Humility
- Openness to diversity
- Broad knowledge base (i.e. self, family, systems, interconnectedness)
- Can see the forest through the trees
- Constant scanning and prioritizing
- Integrating & connecting
The Ultimate Journal Club was yet another forum in which was highlighted the unique ability of Family Medicine Physicians to address the needs of the current crisis in health care. These same characteristics were repeated in the morning keynote by Dr. Robert Graham who clearly outlined how Family Medicine principles can help improve the cost, access, and quality of health care.
So...it seems like Family Medicine is integral to the future of medicine. Med. students, pay attention. The wind is shifting (almost daily on Capitol Hill) and we've got to be prepared for where we end up.
References
Friday, July 31, 2009
"Lub dub" and so much more - Heart Sounds Workshop
 This afternoon I went to a heart sounds workshop put on by The Toledo Hospital. We used an awesome program called CardioSim that broadcasts heart sounds over a wireless network to these headsets (see pictures.) We started with the basics - which side of the stethoscope to use for which sounds, where to listen, how each heart sound is made, etc. Moving on to murmurs we got to see CardioSim in full action, listening to each murmur with and without lung sounds, at varying intensity levels, and with and without prompted visual cues of the sounds on the screen. We ended with a closed eyes "final exam" and a raffle for a Littman stethoscope.
This afternoon I went to a heart sounds workshop put on by The Toledo Hospital. We used an awesome program called CardioSim that broadcasts heart sounds over a wireless network to these headsets (see pictures.) We started with the basics - which side of the stethoscope to use for which sounds, where to listen, how each heart sound is made, etc. Moving on to murmurs we got to see CardioSim in full action, listening to each murmur with and without lung sounds, at varying intensity levels, and with and without prompted visual cues of the sounds on the screen. We ended with a closed eyes "final exam" and a raffle for a Littman stethoscope.
It was the perfect review for medical students, starting at a slow pace and building to practice with critical skills that we will use everyday. These talks are one of many reasons I love coming to these conferences!!
Exposition Hall = Games, Prizes, and...oh yeah...Residency Programs
Like many conferences, the AAFP NC has an exposition hall that's filled with a constant hum of "shmoozing" conversations, the flash of cheap give-away gadgets, and, every once-in-awhile, a jewel. Booth 1010 is one such jewel. The Center for the History of Family Medicine's booth does not seem to get much action, but something from their table catches my eye. I walk closer and discover the shiny objects in the picture below.
After some time gazing at these historical instruments and chatting with the CHFM's representative, I discovered that there is a rich history of how Family Medicine got to be where it is today - poised to become a unique source of quality primary health care - and there are people actively working to document and preserve that shared story of our profession.
If you want to better understand the future of Family Medicine by better knowing its past, explore the Center for the History of Family Medicine's website. Answer questions like...
- When the first Family Medicine Residency program was introduced to Massachusetts?
- Why is Dr. John Willis considered to be the "Grandfather of Family Practice"?
- How old is the specialty of "Family Medicine?
Oh...and if you can guess what the instruments were used for, you get a prize! On to the next booth!!
Best FMIG practices
I'm going to try to blog live, macworld style.
---
Edit: if you are actually following this live, refresh the page often.
---
9:37am Oregon Health and Science University is presenting their Baby Beeper program. It sounds pretty cool. Basically, first and second year students get an opportunity to see prenatal and maternity care through the lens of family medicine. Students go to at least one pre-natal visit to meet the mother, and family medicine residents call/beep students when the mother goes into labor. Residents also try to schedule post-natal visits with the students. Needs: a dedicated student coordinator, must establish buy-in from residents and L&D nurses.
9:43am Clarification, beepers are out of style and could be more impersonal. Residents and students exchanged cell phone numbers. Another program OHSU started this year was the "No One Dies Alone" program: students sit with terminally ill patients in the hospital to be there for them.
9:45am Pennsylvania State University won the Program of Excellence Award in Exposure to Family Medicine & Family Physicians. They organized a series of residency dinners wherein FM residents from different programs in the area treated students to dinner in the city to discuss any one of a list of topics that students were interested in.
9:48am Residents in Hershey PA willingly treated students for this dinner series... do you think the Boston residents are up for that?
9:52am University of Nebraska is describing highlights from their procedure night workshops. 3-4 FM residents teach 30-40 students how to do a particular procedure: casting, suturing, lumbar puncture, airways and intubation, ABG's and IV's, elbow injections and lung sounds. Sounds very similar to BUSM FMIG's sports medicine workshop series. Donna Kurowski (MS2) is heading that up this year, so keep an eye out for her emails.
9:56am Sebastian is introducing BUSM FMIG! Marcel and Jen are up...
 9:58am We tackled the challenge of making primary care sexy by strengthening the FM community and by highlighting the diversity of family medicine practice. The latter was especially emphasized during last year's National Primary Care Week. I hope we can have another active NPCW this year, want to help plan events?
9:58am We tackled the challenge of making primary care sexy by strengthening the FM community and by highlighting the diversity of family medicine practice. The latter was especially emphasized during last year's National Primary Care Week. I hope we can have another active NPCW this year, want to help plan events?10:00am NPCW is a great event to co-sponsor with many potential partners on campus. Working together also brings in many students including students who may not necessarily be interested in FM.
10:01am I see Sebastian taking photos from the front, so you'll see pictures here soon.
 10:02am New things for our FMIG last year: newsletter "All in the Family", blog, social events. Marcel just gave me a shoutout in the back as one of the contributing bloggers. Little does he know that I am live blogging their talk.
10:02am New things for our FMIG last year: newsletter "All in the Family", blog, social events. Marcel just gave me a shoutout in the back as one of the contributing bloggers. Little does he know that I am live blogging their talk.10:03am Ok never mind, he does know. Nice, there's a wordle of blog posts up on the powerpoint. 60 blog posts! 800+ visitors to the blog!
10:07am Meharry Medical College won the Program of Excellence Award in Community Service, Special Consideration Award for First-time Applicant. Some improvements that they implemented this year: paid dues for members to encourage commitment, really cool FMIG shirts ($5 each! Must get on that), text reminders about meetings and events.
10:10am Meharry's Project R.E.C.E.S.S. was featured in the Tennessee Academy of Family Physician's Journal (didn't catch the acronym). The project focused on smoking prevention at a local elementary school because the Tar Wars program couldn't get started in time. The featured booths: Gasping for Air activity, Jar of Tar illustration, Hazards & Effects of Smoking which was a black lung model and display board. The prizes were all active toys, such as kites, promoting active lifestyles-- what a great idea!
10:16am Who's up for starting a Tar Wars program in Boston?
10:18am And it's all over. Onto the Exposition Hall!
Main Stage Lecture: Stephanie Vance, Advocacy Guru

How can we be most effective as citizens going to DC to advocate for health care reform?
First time at NC!
Do you remember when we had that discussion: Why is primary care not sexy? I think it was during the Crisis in Primary Care talk last fall. After Dr. Epperly's keynote speech yesterday, I think we can all agree that if primary care was not sexy before, it sure is now. What a great beginning to what is turning out to be a great conference! I definitely think everyone should have the chance to hear Dr. Epperly speak on the current healthcare reform...
Well, guess what?
Dr. Epperly is coming to BUSM in October! More details are coming, but suffice it to say that the FMIG Region 4 Coordinator, our very own Sebastian Tong, cornered Dr. Epperly at NC last year and somehow convinced him into putting BUSM onto his calendar during his trip to the AAFP Scientific Assenbly in Boston!
Yesterday, the first day of the conference, I attended a number of great workshops, my favorite being "Maternal Care and Childbirth." Dr. Scott Stringfield from the Via Christi Family Medicine Residency in Wichita, KS, examined most of the misperceptions surrounding family medicine physicians who practice obstetrics.
I became much more interested in family medicine after learning that family docs CAN deliver babies, and that family docs CAN perform c-sections. Two weeks after my last exam of first-year, I shadowed on the Labor & Delivery floor at BMC for a day. It was so cool, you should definitely do it too. If you didn't know already, at BMC the attending duties on L&D are equally shared by an OB/Gyn physician, a family medicine physician, and a midwife!
However, there are many physicians who will argue that family physicians cannot safely provide obstetrical care for a myriad of reasons such as inadequate training. Dr. Stringfield encouraged all of us to examine the data and to look at existing family medicine residency programs that include extensive OB training.
Family Physician OB Stats from the presentation:
- In 1987 41% of family physicians did OB in practice
- 22.9% family physicians doing OB (range 8.0 – 45.4 %)
- Highest region – West North Central @ 45.4% (IA, KS, MN, mo, NE, ND, SD)
- 7.3% family physicians do c-sections (range 0.8 – 11.1 %)
- 4% of FM privileges denied (usually related to OB)
- Highest area of restriction – New England region 4.9%
- Studies show that family physicians deliver 23% of America’s babies!
Thursday, July 30, 2009
Wilderness Medicine and Outdoor Health
After a brief discussion reviewing the primary and secondary trauma examination surveys (the first for the unconscious, disoriented, unstable patient or one with multiple injuries and the second for a more detailed exam of the pertinent injuries on a stable patient), we broke up into four groups to work on some hands-on skills.
In the first group, we discussed open versus closed trauma and their general management, as well as when to treat an injury and keep hiking versus when to pack out. In the second group, we practiced using various items you may have at a campsite to immobilize and brace a leg, for example using a camping pad and clothes to splint a leg from above the knee to below the ankle.
In the third group, we practiced "unfolding people", safely moving them from positions you find them down after an injury in, back to a neutral position that would make it easier to carry them away from the site. Too bad we didn't have a camera with us at this session; you could have seen your own Jen Hsia professionally unfold me.
Fittingly, in the last group we practiced various ways to carry injured people. We were challenged to come up with ways to carry people alone (piggyback, fireman's carry, allowing them to lean on you) and with a partner (shoulders and ankles, allowing them to brace between you.) One of the best answers was to form a chair out of your and your partner's arms forming a square base. We also experimented to figure out the best way to use a tarp and two long sticks (if you have them) to carry someone out. We decided the best way was to place the sticks on the 1/3 lines of the tarp, folding the tarp over them, using the person's body weight to hold the free ends down.
Overall, it was a great workshop, mixing in some teaching with hands-on practice of some very helpful techniques. It was also nice to see the CMMC people again. They come down about once per year to teach workshops like this at BUSM for the FMIG and some students (myself included) elect to spend their 6 week core Family Medicine rotation up at CMMC in Lewiston, ME.
What Medical Students Can Do for Health Care Reform
Taking care of business...

While the National Conference for Family Medicine Residents and Students features a multitude of workshops and lectures, there are important "business" meetings that occur in the background. These meetings of the Resident and Student Congresses produce recommendations and actions that range from...
"Recommending that the AAFP express condolences to the families and communities of physicians and their advocates murdered while providing patient care."
to
"Recommending the AAFP strongly promote bicycle helmet usage..."
to
"Recommending that the AAFP strongly encourage the individual constituent chapters to develop preceptorships in underserved areas for all medical students."
This afternoon, I sat in on a 2-hour orientation session where members were nominated for different representative positions, current officers gave updates from the many different boards and committees, and AAFP reps gave an overview of the resolution development process. In all it was remarkable to see the underpinnings of the operation of a large professional organization. How does one reach consensus statements? Where do new ideas come from? This session laid the groundwork for these procedures and I hope to see how they play out tomorrow and Saturday.
After the orientation, student and resident members broke out into smaller topic-based discussion groups on issues surrounding Minority Health, Underserved Populations, Rural Health, Medical Education/Curriculum, Legislature/Public Policy, and more. I sat in on the Legislature/Public Policy discussion - understandably one of the more popular groups this year - and heard about current health reform efforts from those who are intimately involved in the process. It was fascinating to hear the mechanisms and politics involved in the process of shaping different health care bills. At the same time, it was incredibly empowering to know that senior-level officers from the AAFP (present at the discussion) were very interested in us producing resolutions that expressed our opinion on things like the current ideas of a public insurance option.
That's all for now! More from the halls of the Kansas City Convention Center later!
Keynote Speaker: Ted Epperly, MD, FAAFP

Dr. Ted Epperly, the AAFP President and Program Director of Family Medicine Residency in Idaho, spoke eloquently about health care reform at this specific time. He called our current health care system the “perfect storm:” 20 million uninsured, businesses that can’t afford to provide employees health care any more. He believes that the current economic crisis and President Obama will come together to create change in our health care system! For example, the first law that President Obama signed into law on becoming President was S-CHIP providing health care to uninsured children.

Ted Epperly, MD, FAAFP, AAFP President addressing students and residents
He explained things that are being presented in Washington DC currently. President Obama has been engaging different groups stating that:
- The status quo is not acceptable
- Each group must give at least a bit in their position.
- We must have reform this year!
He said that President Obama believes strongly in family medicine and primary care. He recounted a recent town hall meeting on health care reform where he was the only person called on by name by President Obama, not as an individual but as a representative of family physicians and primary care doctors. Dr. Epperly reiterated to the President that reform cannot happen unless we have a primary care backbone to that reform. He argued that “Fixing primary care is fixing the health care system.”
The current system is failing the American public. Medical schools are producing 90% specialists and 10% primary care doctors. We need 50-50 to serve the American people. Medical schools don’t get it: they are producing doctors to function in specialty hospitals and academic centers. The public needs primary care doctors who will serve in the community and serve the people.
The World Health Organization stated this year that each good health care system must be founded on a good primary care system! This was pushed by the American contingency led by the HHS Secretary.
The AAFP is playing a key role in these health care reforms. If the AAFP is not at the table then they are on the menu! The health care reform is changing not by the day but by the hour! We have a great advocate for Family Medicine in President Obama!
This is an exciting time to be a part of family medicine and primary care given all the health care reform - throughout the conference, we will be finding out about more opportunities to get involved with this health care reform in this exciting time in health care reform history!
Student asks question of Ted Epperly, MD, FAAFP
*Read our earlier post on Dr. Epperly's contribution to the White House Health Care Summit back in March 2009.
Welcome to Kansas City - AAFP National Conference for Medical Students and Residents

Good morning from Kansas City! Today is the first day of the 3 day National Conference for Medical Students and Residents. Over the next three days, we will be posting regular updates on the Blog about different sessions and workshops at the conference. Keep checking in regularly for updates and to hear about what’s going on!
Saturday, June 20, 2009
The High Cost (and Poor Quality) of Health Care: Blame it on the C-c-c-c-c-capital-ism?
“Come on,” the general surgeon finally said. “We all know these arguments are bullshit. There is overutilization here, pure and simple.” Doctors, he said, were racking up charges with extra tests, services, and procedures.This is the hook to surgeon-writer Atul Gawande's recent article in The New Yorker about the causes of health care costs in the USA. For this article, he traveled to McAllen, Texas, whose expenditure on health care is second only to Miami. On the ground, he spoke with physicians, hospital administrators, local business persons, and working-class residents. His research and conversations indicate that the principle reason for increased health care expenditure is that physicians in McAllen are systematically overusing medicine.
Physicians as Gatekeepers
If we look at the distribution of health care expenditure (below), physicians control the majority of decisions about expenditures...and rightly so. After all, shouldn't trained healers be the ones working directly with patients to determine the appropriate services to provide?
 Source: Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group.
Source: Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group. Despite this key role, however, gatekeeper physicians have received relatively little attention/scrutany until recently. Drug companies, insurers, hospitals, and medical device manufacturers traditionally dominate the national conversation. Gawande reminds us of the central role that physicians play in the health care system - for better or for worse.
Health-care costs ultimately arise from the accumulation of individual decisions doctors make about which services and treatments to write an order for. The most expensive piece of medical equipment, as the saying goes, is a doctor’s pen. And, as a rule, hospital executives don’t own the pen caps. Doctors do."Blind Spots": Personal Bias in Medicine- Atul Gawande, "The Cost Conundrum"
At the Second Annual (Student-run) Cultural Competence Workshop at BUSM, Prof. Linda Barnes spoke about cultural "blinds spots" that physicians may bring into the patient room. She mentioned biases with regard to cultures of race, class, gender, education, nationality, BMI, etc. But why does this matter? Most people would contend that very few physicians are outright "racist" or "sexist." The impact of subconscious "blind spots", however, is subtle and often occurs when medical decision-trees are less clearly defined. One example from Gawande's article describes a study done on physicians from high- and low-expenditure cities who were given sample patient cases with a ranging degree of established treatment protocols. They found that...
...in cases in which the science was unclear, some physicians pursued the maximum possible amount of testing and procedures; some pursued the minimum. And which kind of doctor they were depended on where they came from.So what is it about place (high- or low-expenditure city) that is related to use of medical services? A comparison between McAllen and El Paso, Texas - a city with similar demographics and significantly lower health care expenditure - indicates that this difference is unrelated to physician training, patient needs, availability of technology, or physician incentive structures. So what is the X factor?- Atul Gawande, "The Cost Conundrum"
Economic Culture
About fifteen years ago, it seems, something began to change in McAllen. A few leaders of local institutions took profit growth to be a legitimate ethic in the practice of medicine. Not all the doctors accepted this. But they failed to discourage those who did. So here, along the banks of the Rio Grande, in the Square Dance Capital of the World, a medical community came to treat patients the way subprime-mortgage lenders treated home buyers: as profit centers.Rather than a culture of race or gender influencing medical decision-making, Gawande posits that a culture of profiteering took hold in McAllen and, furthermore, threatens to dominate the national health care scene. The reason that this culture permeated McAllen is a combination of individual actions and systemic context. In a health care system that compensates quantity over quality and that promotes individualism/fragmentation over teamwork, individual revenue-leaning physicians were easily able to shift their behavior from using only necessary labs & procedures to using the maximum possible.- Atul Gawande, "The Cost Conundrum"
How to Transform a Revenue-focused Culture to a Healing-focused Culture
While McAllen may be an outlier, it represents an extreme that has the potential to spread throughout the current health care system, further-sending health care expenditures through the roof. Fortunately, in better defining the nature of the issue in terms of medical culture, Gawande implicitly points us in the direction of a solution: cultural re-shifting towards collaborative, quality-driven medical care. In designing a cultural shift, one must do at least three things:
- Establish principles of the "new" culture
- Create mechanisms for turning these principles into action
- Disseminate the principles and mechanisms to the target market (ex. physicians)
1. Establish principles of collaboration, quality-focused and patient-centered health care.
It seems that in our current state of high-cost, low-quality health care, we have spend much of our energy on cost-containment - this being the mantra of current health reform efforts. This seems consistent with the philosophy of W. Edwards Deming, a management consultant who "made a significant contribution to Japan's later reputation for innovative high-quality products and its economic power" (Wikipedia), who noted that when organizations focus on cost, then over time costs rise and quality falls. On the flip-side, however, when organizations focus on quality, then quality improves and costs fall. Although simplistic, this philosophy is echoed by Prof. Michael Porter, an expert on competitive strategy who recently focused his attention on competitive environments in health care. Porter (2008) states that in order to be successful, health reform must be guided by three principles:
- A common goal of value for patients (i.e. patient-centered)
- Medical practices organized around conditions and care cycles (i.e. collaborative)
- Measurement of results (i.e. quality-focused)
2. Develop mechanisms for implementing the principles of good care.
Delivering health care based upon the principles of collaboration, a focus on quality, and patient-centered care is a challenge given the fragmentation and quantity-focus of current policies. The PCMH is an attempt to implement the guiding principles within the current system. This following video from the AAFP describes how, by combining traditional primary care and family medicine with modern technology, the PCMH has already been integrated into existing clinics and has produced better health outcomes, improved physician job satisfaction, and reduced costs. Satisfied early-adopters include IBM, which had the following endorsement: "IBM believes that the Patient-Centered Medical Home addresses the core issues of what's lacking in health care."
3. Actively promote adoption of principles and mechanisms
How does one engineer a culture shift? One answer lies with the experts of massive behavior influence: Coca-Cola, Philip-Morris, Nike, etc. In promoting a culture shift, these organizations use active approaches at multiple levels to meet their goals of maximizing revenue: lobbying for public policies, focused marketing campaigns, word-of-mouth, and more. In the realm of public policy-making, however, these ideas have lagged far behind the private sector. Only in 2008 was the term "culture change" with regard to public policy coined by Knopf et al. in their paper, "Achieving Culture Change: a policy framework." Knopf et al. integrate ideas from behavioral economics - a field that combines human and social sciences (esp. with decision-making theory) with economic models - with traditional policy-making theory (ex. incentives, regulations and legislation) to describe multi-level approaches to enacting more effective public policy. In effect, they are adopting the strategies of the private sector.
However, while Knopf et al. describe both society-wide (ex. economics, media, & law) and individual (ex. peers, family, community & workplace) influences on culture change, Gawande seems to point out that in our current discussion of health care reform, individual-level influences (i.e. "anchor-tenants") are being left out. In his popular book, "The Tipping Point: How Little Things Can Make A Big Difference," Malcolm Gladwell explores the nature of how individual-level actors can create epidemics of products, ideas and behaviors (ex. AYBABTU). In relation to the innovation diffusion curve (below), Gladwell describes three major agents that can drive an epidemic:
- The Maven - collectors of knowledge. They are the "early adopters" in the Innovation Diffusion Curve below and constantly have their ears on the ground.
- The Connector - knows a lot of people. They take innovations and disseminate them to the right people.
- The Salesman - powerful persuaders. They help bring an innovation from early adoption to larger diffusion.
How can one reach the Mavens, Connectors and Salesmen of the proposed epidemic of quality-driven medical care? Much like pharmaceuticals target key enzymes (i.e. "hubs," the Kevin Bacon's of the cellular world), the promoters of the culture shift must specifically target Gladwell's agents of change. The well-organized and broadly-based medical societies (ex. AAFP, AMA, APS, etc.) offer one potential route for specific targeting. They have identified leadership and local chapters that can quickly disseminate and gather information. These chapters have the ability to administer brief surveys to their members that could identify the potential change agents in their community of physicians (ex "How many physicians do you have weak ties with in your community?", "How many medical journals do you keep updated on?", etc.). Once these individuals are identified, local or regional chapters can host workshops designed to empower these agents of change to develop an intentional culture of collaborative, quality-focused and patient centered medical care. This is the most effective way of using few resources to have the greatest impact on individual level elements of culture. The time for health reform is now, and, as Gawande warns, even if we improve finance structures, if we don't address physician culture, we could still see trends of higher expenditure and lower quality.
The decision is whether we are going to reward the leaders who are trying to build a new generation of [collaborative and quality-focused solutions]. If we don’t, McAllen won’t be an outlier. It will be our future.What do you think?
-Atul Gawande, "The Cost Conundrum"
- Are physicians really responsible for high-expenditure in health care?
- Can the PCMH address issues of quality-improvement and cost-reduction?
- If so, is a cultural change possible?
- Do we have a right to "engineer" culture change at an individual-level or is it up to traditional policy?
- Do physicians (as a social group) have a responsibility to improving society-wide health?
References
- Bein B. "PCMH Gets Off to Slow Start in Nation's Medical Schools." AAFP News Now. 2009.
- Gawande A. "The Cost Conundrum." The New Yorker. http://www.newyorker.com/reporting/2009/06/01/090601fa_fact_gawande
- Gladwell M. The Tipping Point: How Little Things Can Make a Big Difference. Little Brown. 2000.
- Knott D, Muers S, Aldridge. Achieving Culture Change: a policy framework. 2008.
- Landau E. "Life expectancy could be topic in health care debate." CNN. http://www.cnn.com/2009/HEALTH/06/11/life.expectancy.health.care/index.html#cnnSTCText
- Porter M, Teisberg EO. "How Physicians Can Change the Future of Health Care." JAMA. March 14, 2007.
- Stange KC. The Problem of Fragmentation and the Need for Integrative Solutions. The Annals of Family Medicine (2009) vol. 7 (2) pp. 100-103
- Wikipedia contributors. W. Edwards Deming. Wikipedia, The Free Encyclopedia. June 18, 2009, 01:36 UTC. Available at: http://en.wikipedia.org/w/index.php?title=W._Edwards_Deming&oldid=297073705. Accessed June 18, 2009.
Thursday, June 11, 2009
Upcoming National Conference
 It's not too late to sign up for the AAFP National Conference for Medical Students and Residents! Family Medicine is the only specialty to have a conference uniquely focused for medical students. The conference includes:
It's not too late to sign up for the AAFP National Conference for Medical Students and Residents! Family Medicine is the only specialty to have a conference uniquely focused for medical students. The conference includes:- lectures from key speakers on health policy (this year's theme)
- workshops and break-out sessions on a vast range of topics. Click here for a pdf with workshop details.
- hands-on physical and procedural workshops
- residency fair with over 300 FM residencies nation wide (tons of free stuff)
- student congress sessions
- chance to network with other students interested in FM and primary care!
Register before July 1st to save $50 on registration. Talk to Dr. Joanne Wilkinson for funding: the Dept of FM/SCOMSA/Mass State Chapter of Family Physicians provides funding for BU students attending!
Tuesday, June 9, 2009
BU FMIG awarded Program of Excellence Award!

This just in...
Our FMIG won the national AAFP Program of Excellence Categorical Award for Promoting the Value of Primary Care. 10 overall and 4 categorical awards are offered each year. The award aims to promote family medicine and share ideas nationally with other FMIGs. This is the first time BU's FMIG has been awarded the PoE award!
Click here to check out other award winners or read our application/accomplishments this year.
Monday, May 4, 2009
Lunch with 4th years
How did you decide to go into primary care; when did you make that decision?
With experiences before coming to BUSM like being in the Peace Corps and volunteering in urban shelters, most of the students knew from the beginning that they wanted to be in primary care. The family medicine clerkship at BU was also a great experience. One of the 4th years initially wanted to do surgery, until he finished the surgery clerkship and realized that it was not for him-- all that getting-up-early and standing-all-day business. He's now going into pediatrics with an interest in neonatology.
International away rotations: how many, and which clerkships can count?
In 4th year, you can do up to 3 away electives. Loophole: there are "inside away" electives, which are programs that are not here at BU, but that are credited and count as though you did it here. So, you could potentially do up to 4 months away, plus an additional 2 months of vacation/interview time... you could be away from Boston for 6 months! You can do away rotations for any of the clerkships if you find the right programs. One of the 4th years did the ER clerkship in Chile and the Family Medicine clerkship in Lesotho!
Did ICM affect your decision for residency?
Short answer: no. Longer discussion: the students shared that in such a big hospital setting, you will run into residents and attendings in the various clerkships who may look down on primary care. That can be discouraging, but it also brought the students who were interested in primary care closer together with shared experiences.
What do you wish you had known before starting third year; general advice?
In all your clerkships, keep an open mind. You may be surprised by what you enjoy, what you are good at, and what you do not like. In your clerkships, push push push for what you want to do and learn. As the youngest member in a large team setting, it is easier to stay in the background, but if you are proactive in your education, you will have many more opportunities to do and to learn. Arrive 5 minutes early and quickly review the patients who were admitted overnight to be more prepared when you round on the patients! When things are difficult, remember that each clerkship is temporary and short, and you WILL get through it. Don't take mean comments personally if it happens. Know that you are getting excellent clinical training at BU.
Which third year clerkships are better to do at BMC instead of the other sites?
Medicine, surgery, and pediatrics were highly recommended to do at BMC. And the fourth years all advised that the order of your clerkships in 3rd year does not really matter-- except that doing medicine before surgery will be really helpful. One tip was that new residents start in June/July, so you may have less chances to do procedures compared to the end of the year in April/May. Another tip: your sub-internship grades are important, and there are many sub-i choices.
Favorite part of your clinical years in med school?
Sub-I. By that point, you do feel like you know what you are doing, and it's fun. Doing a rotation at an Indian Health Service, a completely different experience. Going abroad for electives.
Lastly, remember to eat something before going into the OR lest you pass out!
New FMIG leaders
The new FMIG leaders for the upcoming year are:
- Caitlin Christie
- Carly Grovhoug
- Donna Kurowski
- Erkeda DeRouen
- Jessica Chi
- Lucas Thornblade
- Neetu Srivastava
Friday, March 27, 2009
The Match and Primary Care
This photo was featured in the New York Times.
Each year, on March 19, thousands of medical school seniors receive their long-awaited match results indicating which residency they will attend. So how did Family Medicine fare this year?
At BUSM, Family Medicine matches held relatively steady, while nation-wide numbers were down. 9 students matched in family medicine this year (down from 10 last year). Match sites included:
- Boston University
- Swedish First Hill, Seattle
- Swedish Cherry Hill, Seattle
- Middlesex, CT
- UCSD, CA
- Contra Costa, CA
- Brown University, CA
- BU: 26 percent of 150 students (17 percent last year)
- Harvard: 10 percent of 165 students (12 percent last year)
- Tufts: 18 percent percent of 104 students (17 percent last year)
- UMass: 39 percent of 100 students (35 percent last year)
Why do more medical students not choose family medicine? A recent report from the Graham Center showed that more medical students would choose careers in primary care if schools were to (1) increase student recruitment from rural and medically-underserved areas and (2) provide long-term experiences in primary care.
Do you agree? What do you think should be done to increase the number of students entering family medicine?
References









